Master Your Swing: The Vital Role of Core Strength and Mobility for Golfers
Posted on April 9th, 2024 by Andries Lodder

Introduction:
It is essential to recognise the critical role that core strength and mobility play in optimising performance on the golf course. Whether you’re a seasoned pro or a weekend warrior, investing in your core strength and mobility can make a significant difference in your game.
The Importance of Core Strength:
- Spine Stabilization – this allows for greater power generation and control, allowing you to strike the ball better and more consistently by ensuring you maintain proper posture and alignment throughout your swing.
- Improved Balance and Stability – this allows you to stay more stable throughout your swing for more accurate and consistent shots. Improved balance and stability reduces unwanted swaying or movement during the swing, resulting in more controlled shots.
- Increased Transfer of Energy for the body to the club which may allow for greater clubhead speeds, helping you to hit the ball further.
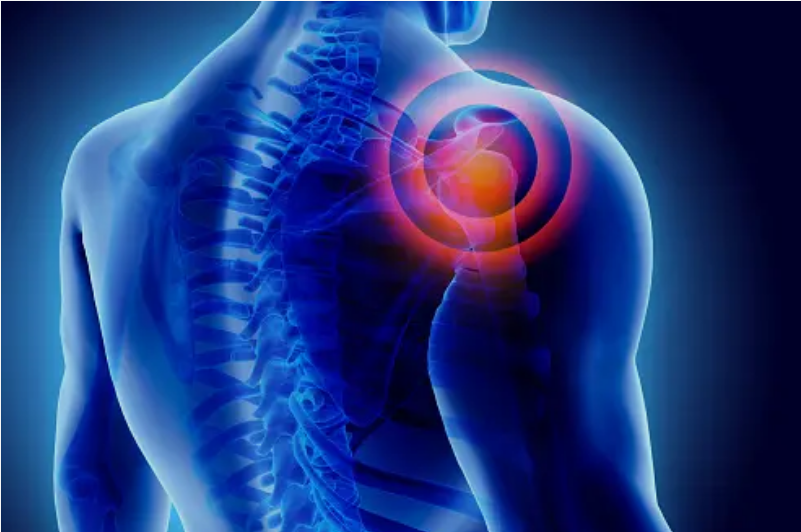
- Prevent Injuries – weakness or imbalances in the core muscles can lead to compensatory movements and excessive strain on other parts of the body.
- Improved Power and Distance by increasing achievable clubhead speeds.
- Endurance and Stamina – golf is a physically demanding sport that requires endurance and stamina, especially during long rounds or multiple days of play. A strong and resilient core helps maintain proper posture and stability throughout the round, reducing fatigue and allowing you to perform at your best from the first tee to the final hole
The Importance of Mobility:
- Full Range of Motion – your range of motion directly influences your ability to achieve proper posture and movements required for an effective golf swing. A lack of mobility in key areas such as the hips, thoracic spine (upper back), and shoulders can restrict your range of motion and compromise your swing mechanics.
- Promote a More Fluid and Efficient Swing – this will allow you to strike the ball more accurately, harder and more consistently – maximising your ability to play the game.
- Improve Form and Technique – appropriate mobility allows you to achieve better technique and positions during your swing, leading to greater clubhead speeds and the ability to hit the ball further more consistently.
- Prevent Injuries – a lack of mobility can restrict your ability to rotate the body. This can lead to compensatory movements which may result in overuse injuries or excessive lateral movement. This may reduce the consistency of your swing, and can result in reduced distance and accuracy.
How to Enhance Core Strength and Mobility:
- Core Strengthening Exercises – Incorporate exercises that target the muscles of the core, including the abdominals, obliques, lower back, and hip flexors. Effective exercises include planks, Russian twists, bird-dogs, and medicine ball chops.
- Flexibility and Mobility Work – Perform dynamic stretching and mobility drills to improve flexibility in the hips, thoracic spine (upper back), and shoulders. Focus on movements that mimic the golf swing to enhance range of motion and fluidity in your swing mechanics.
- Balance and Stability Training – Incorporate balance exercises, such as single-leg stands on the Airex mat or bosu ball exercises, to improve proprioception and stability throughout the swing. Better balance translates to improved weight transfer and control during the swing sequence.
- Functional Training – Engage in functional exercises that simulate the movements and demands of golf, such as rotational exercises with resistance bands or cable machines. These exercises help reinforce proper movement patterns and muscle activation specific to the golf swing.
Conclusion:
Whether you’re striving for longer drives, more consistent ball striking, or injury prevention, a strong core and appropriate mobility are key to achieving your goals and enjoying the game to its fullest. Consulting with a Biokineticist for a comprehensive assessment, as well as an individualised exercise program focused on the above-mentioned key areas can help take your game to the next level. Please do not hesitate to contact us, we would love to help you improve your golf swing.