Understanding the Posterior Cruciate Ligament (PCL)
Posted on September 30th, 2024 by Andries Lodder
By: Gcina Gumede
Structure and function of PCL
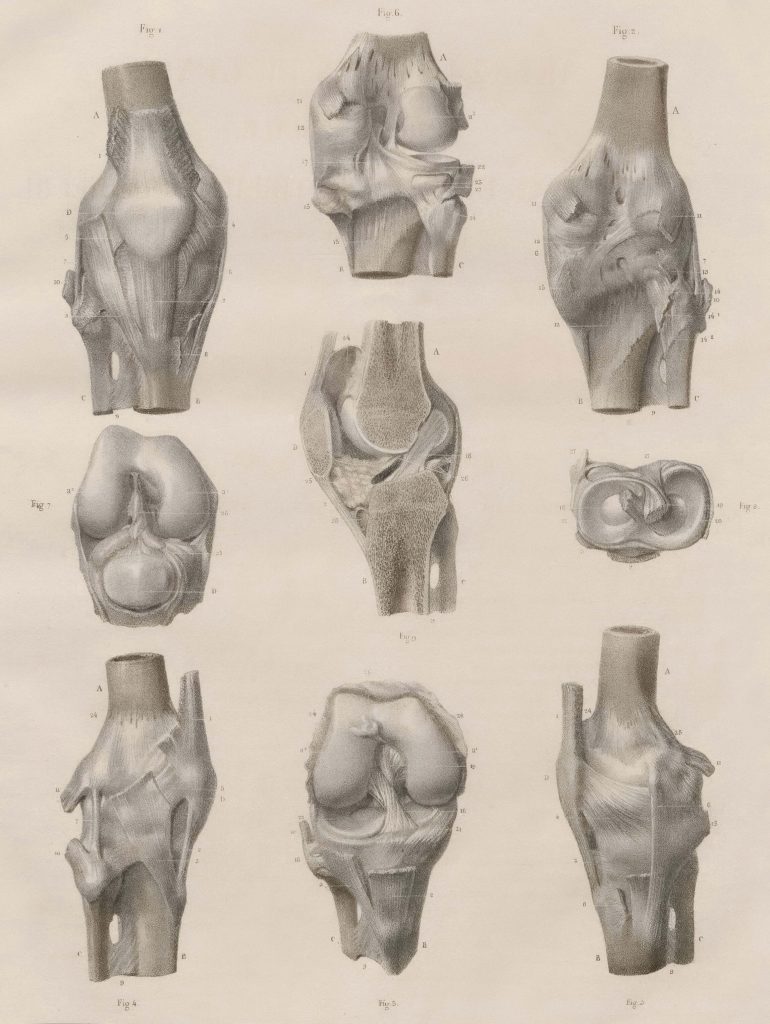
The posterior cruciate ligament is found in the knee just behind the anterior cruciate ligament (ACL). It connects the femur (thigh bone) to the tibia (shin bone) and it prevents the tibia from moving backwards. This ensures that there is smooth movement of the knee joint.
The PCL is comprised of robust connective tissues, including primarily collagen fibers, which are known for their high tensile strength. These fibers are crucial in anchoring the ligament firmly between the bones, ensuring optimal joint stability. The PCL’s primary role is to work together with other ligaments of the knee, such as the Anterior Cruciate Ligament (ACL), to stabilize the knee joint, particularly during dynamic movements such as running, jumping, and sudden directional changes.
PCL Injuries
Injuries to the PCL are often caused by direct trauma or excessive force to the knee. Common causes include motor vehicle accidents where the knee hits the dashboard, sports-related collisions, or falls that result in hyperextension of the knee. Risk factors for PCL injuries often include activities that involve high-impact forces or rapid changes in direction.
There are various types of PCL injuries, classified based on their severity. A Grade I injury involves a partial PCL tear, whereas a Grade II injury indicates a more significant but still partial tear. A Grade III injury is a complete tear of the PCL, and a Grade IV injury involves damage to the PCL as well as other knee ligaments
Symptoms of a PCL injury might include pain, swelling, a noticeable instability of the knee, and difficulty bearing weight. Diagnosis typically involves a combination of physical examination techniques, such as the posterior drawer test, and imaging studies like MRI to confirm the extent of the injury.
Treatment and Rehabilitation
Treatment for PCL injuries depends on the severity of the injury. Non-surgical approaches are often effective for less severe injuries (Grade I and II), and they include rest, ice, compression, and elevation (RICE) to reduce swelling and pain. Physical therapy exercises aimed at strengthening the quadriceps and hamstrings, which help stabilize the knee, are also critical. For more severe or complete tears (Grade III and IV), surgical intervention might be necessary. Surgical options include PCL reconstruction, where a graft is used to replace the damaged ligament. Rehabilitation plays an essential role in recovery post-surgery. This process typically involves a well-structured physical therapy regimen designed to restore knee function, improve strength, and regain full range of motion. The rehabilitation timeline can vary but often includes progressive exercises tailored to the individual’s specific needs and the injury’s extent.
Please feel free to contact us on social media or on our website.