HYPOTHYROIDISM
Posted on February 25th, 2016 by Andries Lodder
HYPOTHYROIDISM
By Dr Kershlin Naidu, Endocrinologist and Specialist Physician, Netcare Waterfall City Hospital
Hypothyroidism is a condition in which the thyroid gland does not produce enough thyroid hormone. It is the most common thyroid disorder.
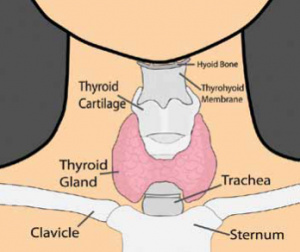
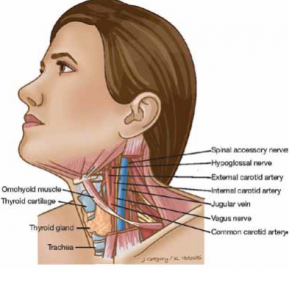
The thyroid is a butterfly-shaped gland in the middle of the neck, located below the larynx (voice box) and above the clavicles (collarbones). The thyroid produces two hormones, triiodothyronine (T3) and thyroxine (T4), which regulates how the body uses and stores energy (also known as the body’s metabolism). Thyroid function is controlled by a gland in the brain, known as the pituitary. The pituitary produces the thyroid-stimulating hormone (TSH), which stimulates the thyroid to produce T3 and T4.
CAUSES OF HYPOTHYROIDISM
In about 95% of cases, hypothyroidism is due to a problem in the thyroid gland itself and is called primary hypothyroidism. However, certain medications and diseases can also decrease thyroid function. In some cases, hypothyroidism is a result of decreased production of the thyroidstimulating hormone (TSH) by the pituitary gland (called secondary hypothyroidism).
Hypothyroidism commonly develops in adult women and becomes more common with increasing age. Thyroid problems generally occur more commonly in Caucasian than in Black populations. However, it can occur at any age and can affect anyone.
The most common cause of primary hypothyroidism is due to an autoimmune disease called autoimmune thyroiditis (Hashimoto’s thyroiditis). The immune system normally makes antibodies to attack bacteria, viruses, and other germs. If you have an autoimmune disease, the immune system makes antibodies against certain tissues of your body.
With autoimmune thyroiditis, you make antibodies that attach to your own thyroid gland, which affect the gland’s function. The thyroid gland is then not able to make enough thyroxine and hypothyroidism gradually develops. It is thought that something triggers the immune system to make antibodies against the thyroid but the trigger is not known. Some people with autoimmune thyroiditis also develop a swollen thyroid gland (goitre).
Autoimmune thyroiditis is more common in patients with:
- A family history of hypothyroidism caused by autoimmune thyroiditis.
- Down’s syndrome. Hypothyroidism develops in 1 in 3 people with Down’s syndrome before the age of 25 years. Symptoms of hypothyroidism may be missed more easily in people with Down’s syndrome, therefore, some doctors recommend that all people with Down’s syndrome should have an annual blood test to screen for hypothyroidism.
- Turner syndrome. An annual blood test to screen for hypothyroidism is usually advised for people with this condition.
- An enlarged thyroid gland (diffuse goitre).
- A past history of Graves’ disease or thyroiditis following childbirth.
- A personal or family history of other autoimmune disorders – for example: vitiligo, pernicious anaemia, Addison’s disease, type 1 diabetes, premature ovarian failure, coeliac disease, Sjögren’s syndrome.
Other causes of hypothyroidism include:
- Worldwide, iodine deficiency is a common cause of hypothyroidism. (Your body needs iodine to make thyroxine.) This affects some countries more commonly than others, depending on the level of iodine in the diet.
- A side-effect to some medicines – for example, amiodarone and lithium.
- Inflammation of the thyroid (thyroiditis).
- A pituitary gland problem is a rare cause (secondary hypothyroidism).
- Some children are born with an underactive thyroid gland (congenital hypothyroidism).
SYMPTOMS OF HYPOTHYROIDISM
The symptoms of hypothyroidism vary widely – some people have no symptoms, while others have dramatic symptoms. These symptoms are notorious for being nonspecific and for mimicking many of the normal changes of aging. Usually, symptoms are milder when hypothyroidism develops gradually.
General symptoms – The thyroid hormone normally stimulates the metabolism and most of the symptoms of hypothyroidism reflect slowing of metabolic processes. General symptoms may include fatigue, sluggishness, weight gain and intolerance of cold temperatures.
Skin – Hypothyroidism can decrease sweating. The skin may become dry and thick. The hair may become coarse or thin, eyebrows may disappear and nails may become brittle.
Eyes – Hypothyroidism can lead to mild swelling around the eyes. People who develop hypothyroidism after treatment for Graves’ disease may retain some of the eye symptoms of Graves’ disease, including protrusion of the eyes, the appearance of staring and impaired movement of the eyes.
Cardiovascular system – Hypothyroidism slows the heart rate and weakens the heart’s contractions, decreasing its overall function. Related symptoms may include fatigue and shortness of breath with exercise. These symptoms may be more severe in people who also have heart disease. In addition, hypothyroidism can cause mild high blood pressure and can raise blood levels of cholesterol.
Respiratory system – Hypothyroidism weakens the respiratory muscles and decreases lung function. Symptoms can include fatigue, shortness of breath with exercise and decreased ability to exercise. Hypothyroidism can also lead to swelling of the tongue, hoarse voice and sleep apnea. Sleep apnea is a condition in which there is intermittent blockage of the airway while sleeping, causing irregular sleep patterns and daytime sleepiness.
Gastrointestinal system – Hypothyroidism slows the actions of the digestive tract, causing constipation. Rarely, the digestive tract may stop moving entirely.
Reproductive system – Women with hypothyroidism often have menstrual cycle irregularities, ranging from absent or infrequent periods to very frequent and heavy periods. The menstrual irregularities can make it difficult to become pregnant; and pregnant women with hypothyroidism have an increased risk for miscarriage during early pregnancy. Treatment of hypothyroidism can decrease these risks.
Myxoedema coma – In people with severe hypothyroidism, trauma, infection, exposure to the cold and certain medications can rarely trigger a life-threatening condition called myxoedema coma, which causes a loss of consciousness and hypothermia (low body temperature).
DIAGNOSIS OF HYPOTHYROIDISM
Blood tests can confirm the diagnosis and pinpoint the underlying cause of the thyroid hormone deficiency. The most common blood test for hypothyroidism is TSH (thyroid stimulating hormone). TSH is the most sensitive test because it can be elevated even with small decreases in thyroid function. Thyroxine (T4), the main product of the thyroid gland, may also be measured to confirm and assess the degree of hypothyroidism.
TREATMENT OF HYPOTHYROIDISM
The goal of treatment for hypothyroidism is to return blood levels of TSH and T4 to the normal range and to alleviate symptoms. The treatment for hypothyroidism is thyroid hormone replacement therapy. This is usually given as an oral form of T4. Generic (levothyroxine) and brand-name (Euthyrox®, Eltroxin®, Synthroid®) formulations are equally effective. However, it is preferable to stay on the same type of T4 rather than switching between brand name and/or generic formulations. If a switch is necessary, a blood test is usually done six weeks later to determine if the dose needs to be adjusted.
Some clinicians prescribe another form of thyroid hormone, triiodothyronine (T3) in combination with T4. Selected patients may benefit from T3 therapy. Depending on the severity of the hypothyroidism, improvement in symptoms may be seen within a few weeks to months after the initiation of therapy.
If you have untreated hypothyroidism:
- You have an increased risk of developing heart disease. This is because a low thyroxine level causes the blood lipids (cholesterol, etc) to rise.
- If you are pregnant, you have an increased risk of developing some pregnancy complications (eg. pre-eclampsia, anaemia, premature labour, low birth weight, stillbirth and serious bleeding after the birth). Women often need higher doses of T4 during pregnancy. Testing is usually recommended every four weeks, beginning after conception. Once the optimal T4 dose is established, testing is usually repeated at least once per trimester. After delivery, the woman’s dose of T4 will need to be adjusted again.
- Hypothyroid coma (myxoedema coma) is a very rare complication. However, with treatment, the outlook is excellent. With treatment, symptoms usually disappear and you are unlikely to develop any complications.
SURGERY
Hypothyroidism can increase the risk of certain surgery-related complications; bowel function may be slow to recover and infection may be overlooked if there is no fever. If preoperative blood tests reveal low thyroid hormone levels, non-emergency surgery is usually postponed until treatment has returned T4 levels to normal.
HYPOTHYROIDISM WITHOUT SYMPTOMS
In some cases, hypothyroidism is extremely mild or causes no obvious symptoms (called subclinical hypothyroidism). The decision to treat subclinical hypothyroidism with T4 is controversial and is dependent on many patient factors. Your doctor will be able to advise you on treatment options.
IN CONCLUSION
Hypothyroidism is a common disorder. Symptoms develop gradually and may be confused with other conditions. The diagnosis of hypothyroidism can be easily made with a blood test. Treatment with levothyroxine is easy, cheap and effective.
Dr Kershlin Naidu
B.Med.Sci(NATAL), MBBCh(WITS), FCP(SA), MMed(WITS), FSEM(SA)
Endocrinologist / Specialist Physician Netcare Waterfall City Hospital
Room SF218, 2nd Floor, South Block.
Tel: 011 304 6865 (emergency on 011 304 6600
Email: drknaidu@waterfallhealth.co.za
Original post of article in Waterfall Estate News Magazine, Issue 4, 2015.
Tweet